|
They are common in developing countries and also seen
sporadically in well-developed countries. Lately the incidence is on the
increase, world over, with the emergence of AIDS. About 60 % of cases are
below the age of 20 years in developing countries. In developed countries
the older people are more commonly affected.
Tuberculomas may occur at any site intracranially.
Infratentorial presentation is more often seen in children. Intrasellar,
CPangle, Optic chiasma, intraosseous tuberculomas have been reported.
Invariably it is secondary from primary elsewhere, more
commonly the lungs, by hematogenous spread.
It has been suggested that the nature of the lesion,
meningitis or a tuberculoma would depend upon the number of bacilli,
their virulence and the state of immunity of the host.
Tuberculomas, more often evolve from tissue reactions,
primarily cell mediated, when the resistance of the patient is high.
Meningitis is seen in those with poor resistance.
About 20% of the patients have multiple lesions.
Most are caused by the human strain. The bovine type is
probably responsible for less than 5 %, especially in Europe. Isolated
cases due to atypical mycobacteria are also seen.
Pathology:
|
Microscopically, there is central coagulative necrosis
surrounded by epitheloid cells, Langhans giant cells(as shown by the
arrow in the picture) and an admixture of lymphocytes and plasma cells.
There may be satellite lesions and perivascular infiltrations.
Tuberculomas vary in size. When near
the surface, some become adherent to the dura, mimicking a meningioma.
The usual type is a well-defined avascular mass with multiple nodular
extensions. It has a pale yellowish, gritty, caseating central core
with a crenated margin, dispersed within an edematous brain, with a
pseudocapsule of compressed gliosed brain.
|

|
In its immature form it consists of small tubercles,
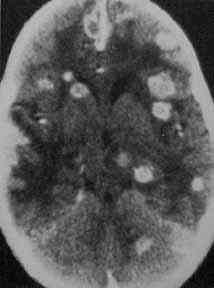
some with caseating or cystic centers, seen as grapelike clusters in a CT
scan.
Occasionally, there are well-localized lesions attached to
the dura with no calcification or caseation. They are called Tuberculoma
en plaque. They simulate an en plaque meningioma.
Tuberculous Abscess does not show the
granulomatous change, but has tubercle bacilli in the pus and resembles a
pyogenic abscess, starting as encephalitis and followed by softening,
leading finally to capsule formation.
Cystic Tuberculomas are rare and have been
reported with the cyst wall confirming the diagnosis.
Calcifications are seen in about 5% and do
not suggest a healed or inactive lesion.
Tuberculuos Encephalopathy is characterized by
obvious edema with varying degree of perivascular myelin loss, attributed
to an allergic reaction to proteins liberated from the lysed tubercle
bacilli. It produces diffuse brain damage, especially in children
.
Tuberculous meningitis in acute stage is
associated with brain edema, increased proteins in the CSF, poor
absorption of the CSF and obstruction to CSF flow. Later it is associated
with tuberculous encephalopathy.In the sub acute and chronic stage, there
is endarteritis affecting the smaller arteries and the large arteries at
the base of the brain may get compressed or occluded due to exudates
resulting in multiple infarcts and basal archnoiditis, which may cause
hydrocephalus and compression of the optic chiasma. Occasionally a tuberculoma
may follow or be associated.
Clinical features:
The patients with a tuberculoma look better nourished unlike
those with tuberculous meningitis. The lesions present, like any other
intracranial SOL, with seizures and / or focal deficits depending on the
location. There may be features of increased ICT.
Diagnosis:
Suspicion is the first step in diagnosis. No diagnostic
procedure either singly or in combination will provide an unequivocal
diagnosis.
The erythrocyte sedimentation rate is often raised. The
mantoux test is generally positive.
A negative mantoux does not rule out a tuberculoma. ELISA
(enzyme linked immunoabsorbent assay) tests of the serum and CSF may be
help.
General investigations should include a search for a
primary.
CT and MRI have helped in early diagnosis and follow-up with
medical management. Multiple lesions are often seen.
|
Imaging:
There is no specific image morphology.
CT: In the early stages,
there may be a small area of increased attenuation surrounded by edema.
There may be contrast enhancing discs or rings with perilesional edema
seen as ‘ fingerlike ‘ projections
Large rings with central lucency as seen in a
pyogenic abscess are also seen. A central nidus may give the appearance
of the so-called “target sign of Welch man”.
A large nodular mass with irregular contours is a result
of small rings and discs coalescing together.
MRI: There is
complete hypo or isointensity or central hyperintensity with a
hypointense rim on T2 and isointensity and / or hypointensity on T1
weighted images. Lipids contribute to low signals on T2. There is
intense enhancement with Gadolinium.
Treatment:
It is essentially medical and surgery may be indicated as
an adjuvant to help inmedical management.
Medical:
When a tuberculous etiology is considered, a stereo tactic
biopsy is performed to confirm the diagnosis. Antituberculous drugs are
started along with steroids to reduce the perilesional edema, if
indicated clinically.
Among the available anti tuberculous drugs rifampicin,
isoniazid, pyrizanamide and streptomycin are bactericidal and the
former three penetrate the blood brain barrier. They form the 1st
line of drugs. After initial treatment with three drugs for three
months followed by any two of the three or isoniazid and ethambutol for
12-15 months. A short course is recommended for better compliance and
claimed to be equally effective.
However many prefer 18 months therapy.
|
Drug:
|
Dosage:
|
Side
effects:
|
|
Rifampicin:
|
10mgms/kg
|
Liver toxicity
|
|
Isoniazid:
|
10mgms/kg
|
peripheral
neuritis
|
|
Pyrizanamide:
|
20mgms/kg
|
Liver toxicity.
|
|
Ethambutol:
|
15mgms/kg.
|
Optic
neuritis.
|
Surgical:
In addition to stereotactic biopsy, surgery may be
indicated when there is
1)
Life or vision threatening increased ICT.
2)
Failure of response to medical therapy.
3)
Persisting hydrocephalus.
4)
Rare presentations such as subdural empyema
5)
FNAC (fine needle aspiration) for skull lesions
|
|

|
|
CT-hydrocephalus
and abscess
|
|

|
|
MRI-Tuberculoma
of the medulla
|
|
|
|
CT-Multiple tuberculomata
|
|

|
|
Basal TBM-MRI
|
|

|
|
Basal TBM-CT
|
|
Total excision, once decided on surgery, is obviously the
procedure of choice in easily accessible lesions. There is no need for
heroic attempts for total excision. Simple evacuation of the pus from a
tuberculous abscess or liquefied caseous material may be adequate, either
stereotactically or by open surgery.
Ventriculo-peritoneal / atrial shunt may be required for
persistent hydrocephalus.
|