|
Brain edema is a clinical problem seen in trauma, tumors, ischaemia, infections and other inflammatory
problems. The term edema was first used to describe the wet and soft
appearance of cut brain at autopsy. The tough and dry appearance was
called brain swelling. The fluid can accumulate either inside the cells
or extracellularly.
Types of brain edema:
Vasogenic
type is due to BBB (blood brain barrier) changes and increased
cell permeability. It is seen in trauma, tumors, inflammation and late
ischemia. The extracellular space is enlarged; later stages the cells
swell as well.
The CSF formation is not increased. Both the white and the
grey matter are affected.
Cytotoxic (brain swelling) type is an
intracellular swelling due to derangement of Na+/K+ pump in the glial
membrane and cell metabolism resulting in Na+ and H2O accumulation. This
is seen in early ischaemia, and medical
conditions such as Reye�s syndrome, intoxication etc.
The BBB is not disturbed. The CSF formation is not
increased. Both the white and the grey matter are involved.
Osmotic type is due to accumulation of excess
water in the brain in response to an unfavorable osmotic gradient as in
water intoxication. The chemical potential of the plasma increases and
water enters the brain due abnormal gradient.
The BBB is intact. The CSF formation is increased. Both
intra and extracellular compartments are affected.
Hydrostatic type is due to movement of
protein-free transudate into the extracellular space due to capillary
dilatation as a result of elevated transcapillary
pressure. Acute arterial hypertension is the usual cause.
The BBB is intact and the CSF formation is not increased.
The edema is confined to the white matter.
Interstitial type is due to acute
elevation of CSF pressure, resulting in periventricular (extracellular)
seepage of water as in acute hydrocephalus.
This is confined to the white matter. The BBB is undisturbed
and the CSF formation is increased.
The differentiation among the above types is artifactual; one type will eventually lead to
another, and considerable overlapping occurs. However, it helps for
better understanding.
Pathophysiology:
The breakdown of the BBB is a central prerequisite to the development
of brain edema. Another basic element associated with brain edema is
energy depletion.
Hydrostatic and osmotic forces encourage the movement of
fluid out of the vascular compartment and into the parenchyma resulting
in mass effect. This compromises the CBF, and the CPP. The ICP increases.
There is abnormal diffusion of nutrients with consequent
acidosis, hypoxia, and inflammatory changes.
Any brain injury initiate a response characterized by
recruitment of inflammatory cells and activation of endogenous substances
also plays a part.
Histamine opens the BBB with
dilatation of pial arterioles.
Bradykinin increases BBB permeability
and enhances blood pressure in the microcirculation.
Excitatory aminoacids (EAA), glutamate
activates many enzyme systems and Ca++ influx, which can result in acute
cytotoxic lesions.
Arachidonic acid is released from brain
tissue in response to neuronal injury. It is the precursor of important
highly vasoactive prostanoid and leukotriene
compounds. Its metabolism through cyclooxygenase pathway generates free
radicals. These radicals induce vasoconstriction of the pial arterioles band venules
without an effect on BBB permeability.
Superoxide radical, hydrogen peroxide, and hydroxyl
radicals are formed from activated neutrophils and metabolites of
arachidonic acid. They cause endothelial lesions with an increase in the
ionic permeability. The radical initiate lipid peroxidation of
glial, neuronal, and vascular cell membranes and myelin is catalyzed. If
severe enough, it causes impairment of phospholipid dependent enzymes and
membrane lysis.
Free calcium is released from its source
by a variety of messenger systems. Glutamate opens the receptor gated
Ca++ channels. Selective neuronal vulnerability in nonvascular brain
lesions, hypoglycemic coma, epileptic seizures, or following brief
periods of ischaemia is calcium related.
Infarction is related to free radicals and acidosis, and the vascular
lesions in stroke are the result of inflammatory reactions involving
calcium, free radicals, and lipid mediators.
Intracellular accumulation of calcium is accompanied by a loss
of free intracellular Mg++, which may directly relate to the extent
of cellular damage, which contributes to secondary injury. Mg++ is
essential for membrane integrity, normal cell respiration, mRNA
transcription, protein synthesis, and also plays a role in glucose
utilization and energy metabolism.
Lactic acidosis due to lactic acid accumulation and
increased pCO2 can denature the proteins and alter the activities of ph dependent enzymes. Lactate enhances brain edema.
Clinical features:
Brain edema alone will not produce symptoms until the ICP reaches a level
that produces local ischemia with or without mass effect.
The symptoms and signs are related to the lesion.
Imaging:
|
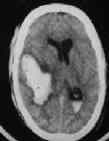
CT: Edema appears as a low-density area
caused by dilution of all constituents of white matter by water. The
decreased amount of lipids, increased proteins and electrolytes leads
to underestimation of the amount of edema fluid based on the
Hounsfield number printout. There is no contrast uptake. Edema is almost always
visible in acute brain abscesses, but rarely in acute intracerebral
hemorrhage. Finger-like projections of low-density areas are
characteristic of a tuberculous abscess. The edema associated with
intracerebral hematoma is located in the cortex and the underlying
white matter whilst in acute subdural hematoma affects
|
|
|
|
CSF seepage in Hydrocephalus
|
|
|
|
both the white and grey matter. Extensive edema suggests
highly malignant tumors.
MRI: It is very sensitive but not
necessarily specific method for detecting lesions in cerebral white
matter and thus brain edema; this is particularly relevant in tumoral perifocal
edema. Prolongation of T2 can be a reflection of a pathological
increase in tissue water and/or demyelination processes.
Post-traumatic perifocal edema
is seen early on T2. 25% of single photon emission computer
tomography (SPECT) scans fail to show alterations in BBB
permeability.
Treatment:
The treatment has three objectives:
|
|

|

|
|
edema - pyogenic abscess
|
Finger-like projections in Tb.ab
|
|
|

|
|
Minimal edema -Ac. hge.
|
extensive edema-high grade glioma
|
|
|
1) Surgical evacuation of masses or CSF
diversion provides an immediate decompression of the intracranial space,
helps to establish a favorable gradient between swollen tissue and CSF
cavities, and washes proinflammatory agents.
Surgery for contusions is controversial.
2) ICP
Control
3) Brain protection:
Energy failure, acidosis, alterations in calcium, cytotoxic
and later vasogenic edema, free radical
formation and excitotoxicity are the events that may lead to irreversible
damage in a cerebral insult.
Brain protective measures aim at increasing the CBF (triple H
therapy), providing adequate blood substrates such as oxygen, and
glucose, and restoration of blood brain interface integrity.
a) CBF augmentation:
Triple-H therapy consists of augmentation of
CBF by means of blood volume expansion, hemodilution,
and pharmacologically induced hypertension.
Hypervolaemic hemodilution
is the first step. The blood viscosity should be maintained between 0.3
and 0.34 hematocrit. If the hematocrit falls below 0.3, packed cells
should be given. Preferred solutions (5% or 20% albumin or fresh frozen
plasma) are those that expand the intravascular space with less
extracellular distribution. It is given in 4-6 divided doses/day, each
administered over 30-60 minutes. Crystalloids remain in the intravascular
space for only 60-90 minutes.
If hemodilution does not produce
the desired result, cardiac output may be enhanced with dobutamine before trying pharmacologically induced
hypertension, which is associated with dangerous side effects.
Pharmacologically induced hypertension may be instituted
only after optimal intravascular volume and cardiac output enhancement.
The systolic blood pressure may be elevated to160mm Hg in a previously
normotensive patient and 180 in previously hypertensive patients.
The triple H therapy is withdrawn gradually starting with
hypertension and later the hypervolaemia once
the desired result is achieved. Dopamine or epinephrine is commonly
used.
The hyperperfusion state of this
therapy should be monitored by the patient's cardiac output through a pulmonary
artery catheter. The CPP can best be monitored with an ICP monitor and
concomitant use of arterial pressure monitor. Frequent laboratory
analyses of the patient's hematocrit provide information on the hemodilution component of therapy. Often, the patient
requires sedation and may also need endotracheal intubation and
mechanical ventilation.
The aim is to keep the hematocrit between 0.3 and 0.34,
hemoglobin to 10-12 gm/dl, serum sodium at 135-145 mmol/l,
serum osmolality at 290-300mOsm/l, and pulmonary wedge pressure at
14-18mm Hg. The CPP is to be maintained over 70mmHg.
Tripe H therapy is an effective therapy for reversing
the neurological deficit, especially in vasospasm associated with SAH and
aneurismal surgery; it is potentially dangerous to other bodily systems.
There is a 25% risk of pulmonary edema and 30% of the patients show
aggravation of brain edema. Anemia and decreased oxygen carrying capacity
are other undesirable side effects.
This therapy is contraindicated in established infarction
and severe brain or pulmonary edema and in anemic patients.
A new strategy aiming to reduce the hydrostatic capillary
pressure using dihydro-ergotamine
combined with a b1-antagonist (metoprolol) and a2-agonist (clonidine)
has recently been described.
b) Attention to energy requirements:
Hyperbaric oxygen therapy has been used in
some centers. This increases O2 concentration in the inspired air and
provides increased O2 to the injured brain. 100% O2 is used widely in pneumocephalus.
Long-term use of O2 therapy may result in acute respiratory
distress syndrome (ARDS).
The blood glucose should be maintained at normal
levels. Tissue acidosis as a result of lactic acid accumulation (due to
anaerobic utilization of glucose), may affect the metabolic recovery.
Ideally the glucose should be maintained at the normal level. There is no
definite evidence to suggest hypoglycemia helps the recovery.
Strict attention to fluid and electrolytes is mandatory. Sodium is the most
important one.
Barbiturates, by depressing neuronal
function, reduce CMR, CBF, and ICP. It has been found effective if given
within 4 hours of the insult. They have profound cardiovascular
depressive effect, which should be monitored.
Etomidate, a short acting anesthetic,
produces similar effects as barbiturates with minimal cardiovascular
depressive effects.
Hypothermia, by reducing CMR, the
release of glutamate and other excitatory neurotransmitters, Ca++ influx,
help edema formation. Profound hypothermia (22-24 degrees C) is
associated with cardiac irritability, ventricular fibrillation, metabolic
disturbances, coagulopathy etc. Mild hypothermia has been found
useful.
c) Restoration of blood brain interface integrity:
Many compounds, most of them currently on trial, are claimed
to stabilize BBB at the endothelial level.
Steroids can inhibit lipid
peroxidation and stabilize lysosomal membrane. Their effectiveness in
post-traumatic and ischaemic edema is not
proven; newly developed synthetic 21-aminosteroids (lazaroids)
lack glucocorticoid and mineralocorticoid activity and are potent
inhibitors of iron dependent lipid peroxidation. Alpha-21-aminosteroids
(U-74006F) appears to have great potentials.
Antioxidants, free radical scavengers, phospholipase
inhibitors have been reported to increase oxygen consumption, glucose
incorporation into amino acids, and phospholipid and GABA synthesis.
Alpha-tocopherol (vitamin E) has beneficial effects on brain edema
and ischaemia. It inhibits both fatty acid
release and lipooxygenase activity and plays a
fundamental role in the stabilization of polyunsaturated fatty acids in
membrane phospholipids. It may also interact with cellular membrane and
prevent peroxide formation by acting as hydrogen donor. Dimethylsulphoxide (DMSO) combined with
mannitol possibly act as specific scavenger for hydroxyl radicals as can ascorbic
acid (vitamin C), glutathione, catalase, superoxide dismutase
(SOD).
Indomethacin induces cylooxygenase
inhibition, modulates arachidonic acid metabolism, and reduces peptidoleukotrienes, which are responsible for
increased vascular permeability leading to edema.
Nimodipine
reduces calcium influx through voltage-sensitive channels; but has the
hazard of producing hypotension. In high doses (60mgm every 4 hour), it
is reported to have beneficial effect on
injured brain. Some studies lately have
found no benefit. Among other compounds trifluoperazine
inhibits calcium binding to calmodulin and inhibits Ca++ mediated K+
efflux at synaptic membranes.
Beta adrenergic antagonists such as propanolol
decrease lactic acid production and reduce edema. The adrenal response
can be reduced by alpha-2- agonist clonidine.
NMDA (N-Methyl-D-Aspartate) antagonists have shown
the greatest neuro protective efficacy of any drug in ischaemia.
Continuing clinical trials are on.
|