|
Dementia is a syndrome
characterized by a gradual onset of symptoms, including memory loss and
decline in such cognitive abilities as thinking and decision making.
Dementia is extremely prevalent in the elderly population, with a severe
dementia affecting approximately 5% of people above 65 years of
age.
Diagnostic features include,
memory impairment and at least one of
the following:
aphasia, apraxia, agnosia, disturbances in executive functioning.
In addition, the cognitive impairments
must be severe enough to cause impairment in social and occupational
functioning. Importantly, the decline must represent a decline
from a previously higher level of functioning. Finally, the
diagnosis of dementia should not be made if the cognitive deficits occur
exclusively during the course of a delirium.
There are many types and causes; the
three major causes of dementia of neurosurgical interest are normal
pressure hydrocephalus (NPH), subdural hematoma, and intracranial mass
lesion. Together, they account for only 3.5% of dementia, most of them
due to NPH.
NPH is discussed in this section.
Normal
pressure hydrocephalus:
NPH
is a state of chronic hydrocephalus in which the CSF pressure is in
physiologic range, but a slight pressure gradient persists between the
ventricles and the brain. There is ventriculomegaly without a rise in
intracranial pressure (ICT) as a result of insidious obstruction of the
CSF circulation due to subarchnoid block. It is also called low pressure
hydrocephalus, occult hydrocephalus, and hydrocephalic dementia. Normal pressure hydrocephalus can be a
reversible or treatable disorder. It is thought to account for about 5%
of all dementias. The incidence is about 1 out of 100,000 people.
Hakim
and Adams first described normal pressure hydrocephalus in 1965.
The NPH syndrome has continued to present many questions with regard to
the most reliable diagnostic and prognostic factors. In addition
the high rate of complications associated with shunting makes treatment
highly controversial.
Etiology:
45%
of the cases are idiopathic and most of the patients are elderly. The
high prevalence of atherosclerotic disease of the cerebral arterioles and
veins vessels has been blamed. Changes in CBF and the CSF chemistry may
play a part. The CSF obstruction may provide the driving force by
establishing a transmantle gradient. The other possible factors are
increased pulse pressure in the ventricles.
The
rest are due to defective archnoid villi. The archnoid villi, and
subsequently subarchnoid pathways, may get obliterated in SAH,
infections, trauma, and intracranial surgery resulting in NPH.
Pathophysiology:
The
exact pathogenic cascade leading to hydrocephalus with normal CSF
pressure and the typical symptomatology is not yet completely understood.
It has been hypothesized that NPH is initiated by an increase in
the ventricular CSF pressure with resulting changes in the tangential and
radial stresses within the brain parenchyma. At first the
ventricular dilatation is small and combined with compensation of the
raised CSF pressure by the compressibility of the low pressure venous
system. As the pressure remains high over hours and days, there is
a net shift of water content from the brain although the water content in
the periventricular white matter increases due to movement of CSF across
the mechanically damaged ependyma under a hydrostatic gradient. The
yielding or plastic deformation of the tissue leads to relaxation of
tangential stresses in the brain parenchyma and consequently to an
increase of subdural stresses. Loss of protein and lipids in the
brain parenchyma occurs due to chronic stress. In this stage CSF
pressure returns to normal values, for instance by decreased CSF
absorption resistance by reopening of previously blocked pathways or new
routes being opened up, or decreased CSF production. The
ventricular dilatation persists due to decreased resistance of the brain
parenchyma. Very small transmantle pressures (2-4 mmHg) are able to
maintain the ventricular dilatation under these conditions.
The
pathophysiology of symptoms in NPH is related to dysfunction of
periventricular structures. This can be explained by the increased
initial tangential stress in this region, the hydrostatic edema which may
occur due to destruction of the ependyma and later on the loss of protein
and lipids. Besides, a pre or coexisting vulnerability of the white
matter caused by ischemia, hypoxia, head trauma and the effects of ageing
may be required for the development of the NPH syndrome.
Clinical
features:
NPH can occur at any age, but is mainly a
disease of the elderly. The occurrence of NPH in children is claimed by
some. Symptoms in children are different from symptoms in the
elderly and include abnormal limb posturing, irritability, and vomiting.
The estimated prevalence among mentally disturbed elderly people ranges
from 0 to 5.6%.
The
important clinical signs are mental changes, urinary incontinence, and
disturbed gait.
Mental
changes:
The
cardinal aspect of the mental change is the slowing of mental processes
without any aberration. Mental deterioration in NPH is due a disorder of
frontal lobe systems which have extensive connections with the basal
ganglia (especially the caudate nucleus), the thalamus (especially the
dorsomedial nucleus), the hippocampus, the amygdale, the cingulated
gyrus, the septal nuclei, and the hypo-thalamus. All these
structures are interconnected by long pathways through the deep white
matter of the brain, most particularly the periventricular regions and
the centrum semiovale. The typical features are a loss of
creativity difficulties with task performance in daily life, poor scores
on tests for formulation and maintenance of strategies, self monitoring
for errors in performance, and ability to ignore irrelevant distracting
stimuli. Problems initiating and sustaining actions may occur. Apathy and
inattention in early stages may precede short term memory deficits.
Akinetic mutism manifests in the late stages.
Gait
disturbances:
Retropulsy,
falling spells, and disturbances of balance may precede a slow, short,
shuffling, wide based, and unsteady gait. The pathophysiology of gait
disturbances is considered to be multifactorial, involving several
periventricular structures such as the corticospinal tract, the caudate
nucleus and its caudatocortical connections with other extrapyramidal
nuclei and the frontal cortex. The gait disturbance is a
subcortical motor control disorder rather than a phenomenon of spasticity
or apraxia.
They
may be bed ridden in the late stages.
Urinary
incontinence:
It
is an important component of the clinical picture. Urge incontinence is
frequently the first sign. The pathophysiology may be related to
dysfunction of the superior frontal gyrus and the anterior cingulated
gyrus. In later stages loss of sphincter control may occur due to
severe frontal lobe dysfunction.
Late
stages there may be faecal incontinence.
There
is no papilledema, but occasionally nystagmus may be seen with increased
tendon reflexes. The primitive reflexes of sucking and grasping appear in
the late stages. Neuropsychological tests of frontal lobe function help
to evaluate the dementia.
Differential
diagnosis:
Occasionally
cerebral degeneration may coexist with NPH and thus present difficulties
in decision making. Some knowledge on other causes of dementia
helps. Dementias can be sub-classified as cortical or subcortical
dementia.
Cortical
dementias often involve aphasias, apraxia, and/or agnosia, and
include, Alzheimer's disease and Jacob-Creuztfeld disease.
Subcortical
dementia is characterized by intact language and visuo-spatial function,
and include Parkinson's, Binswanger’s disease, Huntington’s
disease, HIV infection, and depression.
In
NPH there are no illusions, hallucinations or irrational speech (frontal lobe
inertia).
Brief
notes on some of the causes of dementia are given below:
Alzheimer’s
disease:
Alzheimer's disease is considered the most common cause (50%). Dementia
often precedes gait disturbances and urinary incontinence. There are
features of cognitive dementia in neuropsychological tests. There is
significant cortical atrophy on CT and MRI. Hippocampal atrophy on
coronal CT is related to Alzheimer’s disease and correlates to poor shunt
response concerning cognitive improvement in suspected NPH. SPECT
reveals diminished uptake in temporoparietal
areas.
Vascular
dementia: Formerly known as multi-infarct dementia (MID).
Results from brain damage caused by multiple strokes (infarcts) within
the brain. Symptoms can include disorientation, confusion and behavioral
changes. Vascular dementia is neither reversible nor curable, but
treatment of underlying conditions (e.g., high blood pressure) may halt
progression. There may be superficial cortical and/or deep lacunar
infarcts on CT-scan or MRI. Normal radiology does not rule out
vascular dementia.
Parkinson's disease: A disease
affecting control of muscle activity, resulting in tremors, stiffness and
speech impediment. In late stages, dementia can occur, including
Alzheimer's disease. Parkinson drugs can improve steadiness and control,
but have no effect on mental deterioration.
Pick's disease: A rare brain
disease that closely resembles Alzheimer's, with personality changes and
disorientation that may precede memory loss. There is atrophy of frontal
poles and temporal poles on CT-scan or MRI, and diminished uptake in
frontal lobes in SPECT. It is difficult to differentiate from
Alzheimer’s disease. As with Alzheimer's disease, diagnosis is difficult,
and can only be confirmed by autopsy.
Creutzfeldt-Jakob disease (CJD):
A
rare, fatal brain disease caused by infection. Symptoms are failing
memory, changes in behavior and lack of muscular coordination. These are
features of cortical dysfunction. EEG shows periodic synchronous
discharge.
Lewy body dementia (DLB):
Also
referred to as DLB (Dementia
with Lewy Bodies). A disease recognized only in recent years,
in which the symptoms are a combination of Alzheimer's disease and
Parkinson's disease. Usually, dementia symptoms are initially present
followed by the abnormal movements associated with Parkinson's. There is
no treatment currently available.
Huntington's disease: A hereditary
disorder characterized by irregular movements of the limbs and facial
muscles, a decline in thinking ability, and personality changes. In
contrast to Alzheimer's, Huntington's can be positively diagnosed, and
its movement disorders and psychiatric symptoms controlled with drugs.
The progressive nature of the disease cannot be stopped.
Binswanger's disease: An extremely
rare dementia marked by loss of memory, mood changes, abnormal blood
pressure, and disease of the heart valves or large blood vessels in the
neck. Other symptoms may include tremors, difficulty walking,
incontinence and depression. Binswanger's is slowly progressive, often
marked by periods of partial recovery, and is not at present curable.
There is diffuse periventricular hypodensities and lacunar infarcts on CT
and MRI.
Progressive
supranuclear palsy: There is pseudobulbar palsy and rigidity with
vertical gaze paresis and impairment of convergence. In a later stage
horizontal gaze paresis and downward gaze pareis. On CT-scan and MRI,
there are hypodensities in different anatomical regions such as the
substantia nigra and superior colliculli. In addition, there is atrophy
of mesencephalon and pons, later followed by distension of the aqueduct
and fourth ventricle and atrophy of temporal lobes.There is diminished
uptake in frontal lobes with normal cortical uptake in SPECT.
Depression:
A
psychiatric condition marked by sadness, inactivity, difficulty with
thinking and concentration, feelings of hopelessness, and in some cases,
suicidal tendencies. Many severely depressed persons also display
symptoms of memory loss.
Dementia related to depression,
alcoholism, drug interaction, thyroid and other problems may be
reversible if detected early.
|
Investigations:
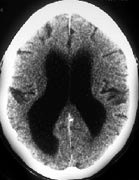
CT scan is the
primary mode of investigation and shows dilated ventricles with normal
sylvian fissures and sulci. Periventricular low density suggests
transependymal flow.
MRI may provide
additional information of the cerebral parenchyma. CSF flow changes may
be studied in MRI. Even if there is some degree of cerebral atrophy,
shunting may help.
Further
tests are normally required if CT and MRI are inconclusive.
|
|
|
|
NPH- CT
|
|
Lumbar
CSF drainage
of about 50ml may help in evaluation; clinical improvement after CSF
drainage implying good response to shunting. This test is not always
reliable, but most commonly employed.
CSF
absorption test,
first described by Katzman and Hussey in 1970, helps differentiate
between presenile dementia and NPH. Saline infused into the lumbar
subarchnoid space at a rate of approximately twice the normal rate of CSF
formation produces a slow rise in CSF pressure in patients with normal
absorption capacity. But when the CSF absorption is delayed as in NPH,
the CSF pressure rises suddenly which predicts good response to a shunt
procedure.
Isotope/contrast
Cisternography
helps to study the CSF circulation. The most commonly used isotope
is iodine 131-labelled human serum albumin (RiHSA). The isotope is
introduced into the lumbar intrathecal space. Normally, activity will
appear within the cisterna magna after half an hour; after about two
hours activity will appear in the basal cisterns and after about 6 hours
over the cerebral hemispheres. By 24 hours the activity is
concentrated in the parasagittal region. Normally visualization of the
ventricular system will not occur. By 48 hours only slight diffuse
activity is generally evident, and symmetry of distribution on
anteroposterior views is the rule. This test is of no use in
non-communicating hydrocephalus. Isotope cisternography in NPH is
characterized by cisternoventricular reflux, lack of isotope in the
anterior basal cisterns, and delayed clearance from the ventricles. Water
soluble contrast, instead of an isotope, helps in a more precise
evaluation.
SPECT scan (single
photon emission computerized tomography) may reveal global diminished
uptake, suggesting a global hypometabolism, in NPH, and help to
differentiate from other causes of dementia.
Xenon
enhanced CT
scan provides a method for cerebral blood flow (CBF) measurement. The xenon
concentration within brain is determined from the CT scans collected
during a 6 minute xenon inhalation. The CT scans enhance with time,
and xenon concentration can be calculated by subtracting the values of
the enhanced scans from the baseline CT. In NPH the regional cerebral
blood flow is decreased in the hippocampal regions and in the frontal and
parietal white matter.
Continuous
ICP monitoring may
predict the outcome of shunt surgery. Those who show transient
increases in ICP (Lundberg B waves) on 24 hours monitoring do well
after a shunt surgery, while those with a flat tracing do not.
Treatment:
CSF
drainage through a ventriculoperitoneal or ventriculoatrial shunt gives
good results. Acetazolamide 250-500/d decreases CSF production and seemed
helpful in one small uncontrolled study. Occasional reports claim no
benefit with shunt.
Some
surgeons prefer to use a low pressure shunt. Others recommend a medium
pressure shunt.
The
mental symptoms improve rapidly and the improvement continues for weeks.
Gait takes a longer time.
In
some cases, improvement after shunting may be delayed for several weeks
to months. In some cases, for unknown reasons, improvement is only
temporary.
On
the basis of numerous studies, in patients with a known etiology and the
complete clinical triad, improvement after shunting will occur in 60-75%
of cases. In idiopathic NPH, this percentage drops to 10-40%.
Postoperative
reduction in ventriculomegaly is not always seen or proportionate to the
clinical improvement. However, there is increased CBF in both grey and
white matter following the surgery.
It
is interesting to note that good outcome following a shunt has been
reported in degenerative brain diseases without all the classical
features of NPH. The presence of atherosclerotic changes does not
influence the results; however, careful selection of patients is
warranted before shunt surgery.
The
following factors suggest a favorable outcome:
1)
Shorter duration of symptoms.
2)
Presence of urinary incontinence and early onset of gait abnormalities.
3)
CT-scan: ventricular enlargement with minimal or absent cortical
atrophy. Enlargement of the third ventricle is also predictive of
good response to shunt.
4)
MRI-scan: A distinction can be made between shunt responsive NPH
(true NPH) and shunt refractive NPH (false NPH) on the basis of T1 and T2
of the water proton of the perventricular white matter. In the true
NPH group both T1 and T2 of the periventricular white matter are
significantly prolonged. In the false NPH group there is only a
significant prolongation of T1. Pronounced aqueductal flow void
extending into the 3rd and 4th ventricle is an
indicator of increased (hyperdynamic) aqueductal CSF flow and shunt
responsive NPH syndrome.
5)
A good response to Lumbar CSF drainage.
6)
Altered CSF dynamics in 24hours CSF pressure monitoring.
7)
CSF levels of delta sleep inducing peptide (DSIP), peptide YY (PYY) and
somatostatin (SOM) are decreased in NPH. Levels of DSIP, SOM and
VIP (vasoactive intestinal peptide) increase significantly in parallel to
the clinical improvement after the shunt operation in NPH patients.
|